A few weeks ago I was having a conversation with my friend’s sister. She works at a fertility clinic, so it seemed like a good opportunity to ask a question that has perplexed me ever since I watched Meet the Parents: Why do men have nipples?
After satisfying my curiosity with an eloquent explanation that touched on evolutionary biology and embryonic development, she raised the stakes.
“Can I ask you a question?” she said. “What do you know about your own fertility?”
For one of the rare times in my life, I had nothing to say. I’ve never given much thought to my personal fertility. Abstractly, maybe — my wife and I plan to have kids one day — but never in concrete terms. Most males, I suspect, are in a similar position.
Fertility has long been viewed as a female issue. Given the biological optics, this is easy enough to understand. Female fertility has visible checkmarks from beginning to end: menstruation, pregnancy, birth, menopause. Male fertility, on the other hand, is much more opaque. We start producing sperm during puberty, and the assembly line continues production until our dying breath. We don’t see it; we don’t talk about it. Until, one day — ideally by design — we find out whether what we’ve been producing all our lives is actually any potent.
This narrative is basically what’s used in Genesis to explain how a century-old Abraham becomes a father, and it captures the average man’s understanding of his own fertility to this day.
But scientific knowledge and medical technology have come a long way since a 90-year-old Sarah gave birth to Isaac.1 It’s telling, however, that societal discourse — at least in western societies — has barely advanced. That’s all starting to change. Shifting demographics, innovations in reproductive healthcare and a burgeoning industry have started to modernize the conversation we’re having about male fertility.
Fertility rates have dropped steeply over the past six decades. According to data from the World Bank, the global fertility rate in 1960 (measured as births per woman) was 5.0. In 2017, that number fell to 2.4. The decline in the United States has not been as precipitous, but it is still striking: 3.7 in 1960 versus 1.8 in 2017.
While many factors have contributed to couples having fewer children, the age at which they are attempting to conceive has played a significant role. The average age of an American woman having her first child in 2018, a CDC report found, was 26.9. That figure surges when filtering for things like education level (30.3 for women with a college degree) and geography (31.3 in Manhattan). For comparative purposes, the average age in 1980 was 22.7.
Dr. Meir Olcha is an OB/GYN who specializes in reproductive endocrinology at the New Hope Fertility Center. I asked him whether this demographic shift has led to higher instances of infertility.
“We know that infertility affects somewhere between 10 and 15 percent of all couples. That number has been fairly stable for at least the past three decades, but some things have changed,” he said. “There are more women today attempting pregnancies at older ages. The failure rate is higher in older women because it’s more difficult to get pregnant as one ages.”
While the public burden of infertility falls almost exclusively on women, the clinical causes are much more evenly distributed. Approximately one in seven couples struggles to conceive. Among those couples, one third of the cases relate to a problem with the male, another third relate to a problem with the female, and the final third represent cases where there is a problem with both. Treatments exist for both sexes, but our collective awareness of them is incredibly lopsided.
“You certainly don’t see a third of marketing geared towards men,” Dr. Olcha said. “I think that’s something about our culture and not necessarily anything about science. You see lots of ad campaigns out there about freezing your eggs, but try to find a campaign that says, ‘Freeze your sperm!’”
Dr. Olcha acknowledges that we’ve come a long way just to achieve the current status quo. “In the 1970s, women didn’t talk about infertility. It would be very taboo to say you had to do IVF to have your child. And yet today, with all the media coverage and social media, women are much more free about talking about fertility, infertility, everything. It’s just a natural part of conversation now. I think eventually that will kick into men as well.”
That’s what a handful of companies and investors are betting on, at least.
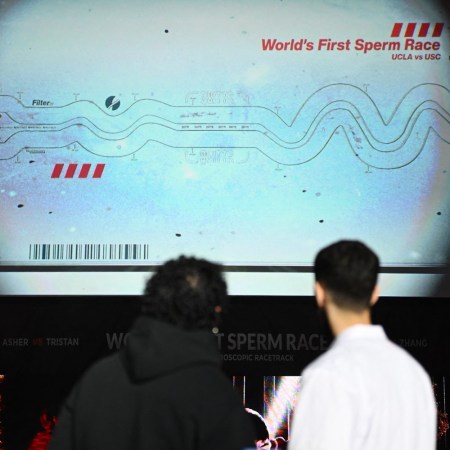
Over the past two years, startups specializing in sperm testing and storage have penetrated the fertility market, demonstrating impressive growth while educating consumers on the oft-overlooked arena of male reproductive health. Legacy, a Harvard-incubated startup founded by Khaled Kteily in 2018, is at the tip of the spear. The company, which recently completed a second round of fundraising, offers at-home testing kits and affordable sperm storage. Raising awareness is a central part of Legacy’s mission. According to a 2017 study published in the academic journal Human Reproduction Update, sperm counts have declined by 50-60% over the past 40 years.
“Men today are about half as fertile as their fathers and grandfathers were,” Sarah Steinle, Legacy’s Head of Strategic Partnerships, tells InsideHook. “On top of that, couples are waiting longer to have children. There’s a growing body of research that shows older men experience fertility decline and also have a higher risk that their partners will have complications during pregnancy.”
Like women, men’s fertility also decreases with age. The cliff isn’t absolute — i.e., there is no male equivalent of menopause — but the scientific evidence is clear: the older men get, the more the quantity and quality of their sperm diminishes. This is why many men are starting to freeze their sperm. Ms. Steinle, who previously worked at one of the leading egg-freezing clinics in New York, believes that society is moving towards a more proactive approach to fertility.
“The process that is used to freeze eggs is called cryopreservation,” she explains. “That was considered experimental until 2013. After that point, once it was proven to be effective, it became much more popular and widely accepted. For that reason, fertility preservation for proactive purposes has become a topic of conversation that people are much more comfortable having in general. Not even as it relates to women — men as well.”
Before sperm is frozen, it is tested. Not to sound repetitive, but fertility testing is something women have been doing for a long time, particularly those actively trying to get pregnant. For their male partners, the increasing prevalence of testing has helped raise awareness.
“The women in those relationships are testing and tracking their fertility. So these men are now becoming aware of solutions like Legacy that are allowing them to do the same. They’re basically testing their sperm in order to get to the root of the issue faster, which saves couples a lot of time, a lot of heartbreak, a lot of money,” Ms. Steinle said.
Legacy offers a range of testing and freezing packages. The sperm analysis is lab-grade, assessing more than 50 data points that evaluate count, concentration, volume, motility (movement) and morphology (shape). As of now, the quality of sperm that is frozen at a traditional clinic compared to a company like Legacy is higher due to a 10-15% decline in motility that occurs when the sample is shipped from a client’s home to the lab. The technology used for in vitro fertilization (IVF), Ms. Steinle told me, reduces the impact of this decline.2
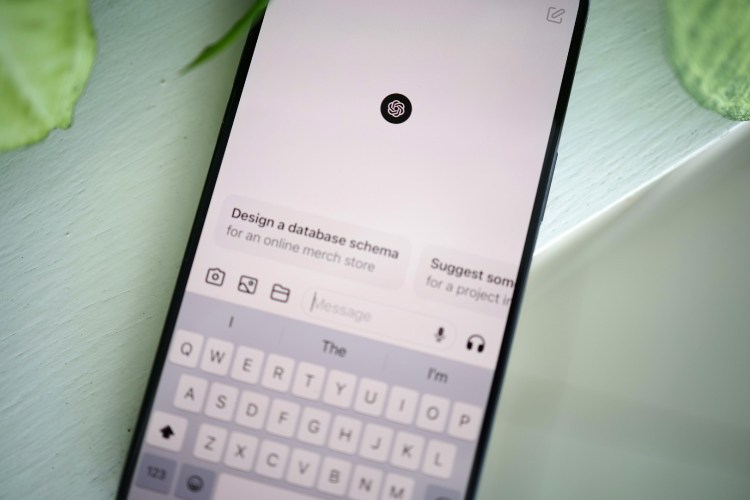
Along with similar startups such as Dadi, Legacy is appealing to clients through an emphasis on affordability, discretion and — most importantly — convenience. The process they promise is simple: a testing-kit is mailed to the client, the client produces a sample in the comfort of his own home, and then he sends it off to the lab in a secure pre-packaged container. Two days later, he receives a detailed testing report. From personal experience, I can confirm that they deliver on this promise.
The FedEx package I received contained a navy-blue box emblazoned with an ornate shield. I opened it half-expecting to find a luxury wristwatch. Instead, I encountered an empty biohazard bag, a soft plastic vial full of a clear yet syrupy liquid labeled “transport media,” an empty plastic lab cup, a pre-addressed FedEx priority overnight package and idiot-proof step-by-step directions. From start to finish, the process was comfortable and easy.3
Two days after returning the package, as promised, I received my test results along with lifestyle recommendations based on a survey I had previously completed. The recommendations felt pretty intuitive, since I already knew that sperm health is starting to be viewed as a biomarker of overall health (for example, the report said I should consider drinking less), but the test results were nonetheless enlightening and comforting. The next time someone asks what I know about my own fertility, I’ll be able to say, “a lot.”
If the test surfaces any kind of alarm bell, customers are encouraged to consult a doctor to determine next steps. Dr. Olcha, the reproductive endocrinologist, has extensive experience in this field. “When we think about male infertility, it’s usually divided into two segments. Either there is an issue with production, or there is an issue with transport,” he said. In other words, two questions are essential to the diagnostic process: Is sperm being produced? And if so, is it being transported correctly from the testicle through the penis?
Though lifestyle certainly affects sperm health, pre-existing genetic conditions are often the underlying issue behind more serious male infertility cases. Men who carry the gene for cystic fibrosis, for example, are usually missing certain parts of their anatomy, such as the vas deferens, the tube that carries sperm from the testicle to the outside world. While a man would know if he had cystic fibrosis — a hereditary disease that affects the respiratory and digestive systems — he wouldn’t necessarily know if he was carrying the gene. This kind of fertility problem is treatable, since the man is producing sperm. Doctors can surgically extract sperm through a process known as TESE.
“The procedure is this,” Dr. Olcha explains. “You open the scrotum, you go into the testicle, and then you dissect out some of the tubules. When you open up those tubules, you find sperm cells. Those are the sperm that we freeze.”
So when, if ever, is male fertility untreatable? “Thankfully a minority of cases,” Dr. Olcha says. These are the cases that involve some sort of production problem typically associated with an underlying genetic condition. One example is Klinefelter Syndrome, a condition in which a man is born with an extra X chromosome, making his chromosomal makeup XXY rather than XY. Men with Klinefelter Syndrome produce little to no sperm.
Microdeletion of the Y chromosome is another condition that’s difficult to treat. “For these men, a piece of their Y chromosome is missing,” Dr. Olcha says. “They look like normal men. They have beards and normal testosterone levels, maybe a bit on the lower side, but they have no sperm production. And those cases are unfortunately very difficult to cure.”
Even in these rare cases, proactive fertility testing offers a clear benefit in terms of managing expectations and gaining an accurate understanding of one’s personal reproductive health. The broader implications of this increased testing and awareness suggest that we’re not far away from a future where the discourse around fertility is considerably more gender-balanced.4 Companies like Legacy are well positioned to facilitate this societal change.
Legacy, which ultimately envisions itself becoming a comprehensive resource for men as they move through the process of fatherhood, has used its business-to-business efforts to help lay the foundations for sperm testing to become a more widely covered employee benefit. Ms. Steinle had a quick response when I asked about any stigma or discomfort involved in the physical procurement of a testing sample.
“It’s our belief that eventually every man between the ages of 20 and 45 will be going through this type of process. It’s easy, it’s affordable, it’s kind of a no-brainer. Men do this on a regular basis anyway, so we call it ‘masturbating with a purpose.’”
Notes
1. Despite these gains, no modern woman has come close to surpassing Sarah’s feat of biblical fertility. Mangayamma Yaramati, a 74-year-old woman from southern India, gave birth to twin girls last September. It’s much more likely that we’ll see Abraham’s paternity record fall in our lifetimes. Ramjit Raghav, a wrestler and farmer who was also from southern India (he passed away last month), fathered a son at the age of 96. In an interview with The Telegraph, Mr. Raghav said, “I credit my stamina and virility to my diet of vegetables and grains.”
2. “When these sperm samples are used [for IVF], it’s typically through a process called ICSI,” Ms. Steinle said. “The doctor will choose one specific sperm in the sample — usually there are millions — so they’ll choose one specific sperm and insert it into the egg in order to fertilize it. For that reason, if there’s a decline in motility, it doesn’t really matter, because the embryologist is the one who is actually picking the sperm.”
3. It did, however, lead to some domestic conversations about masturbation that reminded me of this wonderfully unbearable scene in American Pie. The elegant blue testing box sat on our counter for a week before I was ready. My wife referred to it affectionately as my “splooge kit,” which actually made it feel like less of an elephant in the room.
4. Not to be lost in this discussion is the fact that a woman’s biological clock is still, and will always be, the single most definitive fertility metric. A more in-depth analysis would contextualize declining global fertility rates by examining topics such as the evolving demographics of the workplace, the increasingly prevalent occurrence of households with a female breadwinner, and how these factors have changed the calculus of family planning.
The Charge will help you move better, think clearer and stay in the game longer. Subscribe to our wellness newsletter today.