Real trauma is getting some virtual treatment.
Technology companies are now competing to assert their dominance in a virtual reality healthcare market, which TechCrunch projects will be worth $25 billion by 2021. While tech firms duke it out in Silicon Valley, people are already using VR to fight their own battles inside their mind.
Virtual reality has found nascent uses throughout health care, and one of its most promising applications is for mental health treatment. It’s been successful in treating anxiety disorders, OCD, phobias, and PTSD.
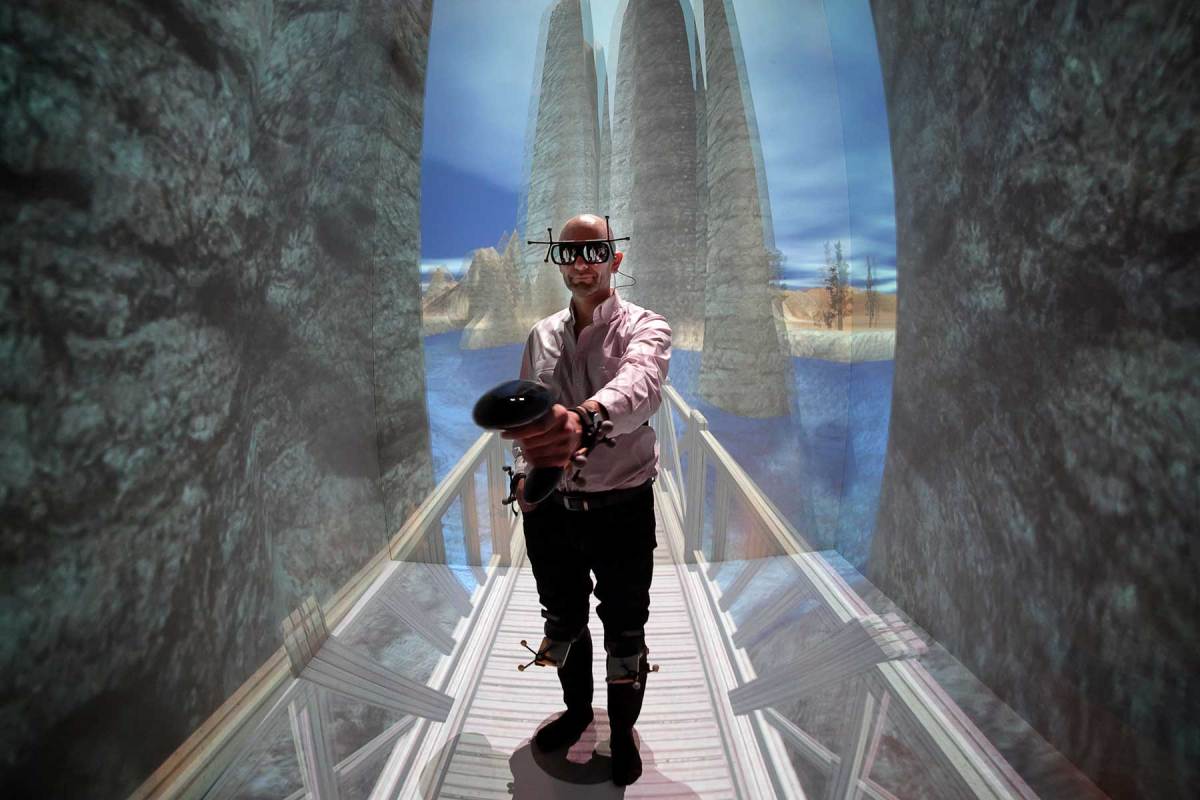
“You can engage patients in these virtual worlds in ways that would be very difficult to do using traditional formats,” Skip Rizzo explained to RealClearLife. He’s the director of the Medical Virtual Reality at USC’s Institute for Creative Technology, where Oculus Rift founder Palmer Lucky was an intern several years ago.
Under Rizzo’s leadership, his team at USC created Bravemind, a VR platform that helps combat veterans overcome their PTSD by reliving their traumatic experiences from Iraq and Afghanistan. The system tries to make the simulation as realistic as possible using scent machines, 3-D sound, and vibrations.
The concept of reliving violence and trauma in visceral detail may sound torturous, but it’s an adaptation of a clinical treatment technique called exposure therapy. Guided by a therapist, it traditionally involves imagining the experience as a way of helping the patient confront, engage, and process it. But, why use imagination when there’s VR?
Bravemind lets therapists customize the details of each battlefield horror to make the exposure therapy sessions replicate a veterans’ personal experience. By tapping into the emotions of that memory, it can help veterans overcome it. In fact, a small 2014 study found that 7 out of 10 patients that used the Bravemind system showed an improvement in their PTSD symptoms by 30 percent or more.
Like many others in the field, Rizzo says VR is so successful with therapy for trauma because it forces patients to confront the emotions that they’ve tried so hard to suppress. Instead just pretending to imagine a scenario, the veteran is right there in his or her memory but with the guided assistance of a therapist. It can also be used on family members of veterans to establish empathy and better understanding.
During VR therapy sessions, patients are hooked up to a range of physiological sensors that measure their heart rate and skin conductance, which can increase during states of stress or arousal. These vitals can help therapists avoid overwhelming a patient too quickly, but they also provide a measurement of treatment progress.
While it’s immersive, patients are introduced to the stressors in stages as they would with conventional exposure therapy. Sometimes they don’t use the VR headset until after several sessions, which is a “safe kind of starting modality” says Dr. Mark Wiederhold, from the Virtual Reality Medical Center. For its centers across the U.S. and Europe (and soon in China), the Virtual Reality Medical Center has developed over 220 VR experiences in-house to treat panic disorders and phobias, such public speaking or claustrophobia.
To treat the fear of flying, the center replicated a true-to-life interior of a Boeing airliner. Widerhold says the patient’s first session usually is just sitting inside the replica. Even once the VR is incorporated, a patient may simulate taxiing before going through the range of stressors in later sessions, from take-off and landing to turbulence or night flights. “You really allow people to develop the skills at their own pace,” Widerhold says.
Without VR, therapists would travel to the airport and possibly even take a flight with the patient as part of their “graduation” from treatment. This that therapists can’t guarantee confidentiality, but more importantly control of the entire situation as they would with VR. “If I have a fear of flying patient, I can guarantee them for this flight we will not have a storm,” explained Jessica Maples-Keller, a postdoctoral fellow at Emory University’s School of Medicine.
“By putting people in environments, I think you can more closely present them with the challenges that they’re going to find in the real world,” Rizzo says. However, Rizzo is quick to point out how helpful VR can be in overcoming challenges other than just PTSD or phobias. For instance, the Medical VR at USC created a job interview simulator for people with autism. By rehearsing in the interview environment with various questions and personalities, they can get accustomed to different scenarios and be emotionally prepared.
It’s used in a similar fashion way with addiction. “You put people that are going through rehab through VR simulations that drive their urge states,” Rizzo says. Someone getting treatment at an inpatient facility might visit a virtual bar or crack house, he says, so they’ll be prepared after they leave the facility.
“With a lot of disorders, we know that people have cues that trigger a desire to engage in some of these behaviors that they’re working on,” Maples-Keller explained. As the lead author of a review on various VR therapies published in the Harvard Review of Psychiatry, she’s familiar with many different applications of the technology. “In the virtual environment, we can sort of bring some of those cues up while they’re in therapy with their provider and work on more effective ways of responding.”
It may seem like a new idea, but virtual reality has been pursued in this realm for the last 20 years. Both the Virtual Reality Medical Center and USC’s Medical Virtual Reality lab have been working on VR since the ’90s, but it was just too limited and too expensive until now.

One of Rizzo’s grad students had taken a prototype with him on an early deployment to Iraq as a proof-of-concept. Even then, it wasn’t until the insurgency picked up in 2004 that the military started to show interest. A year later, Rizzo’s team got their first round of funding. Now, Bravemind is used at about 100 U.S. military facilities across the country. It’s also been adopted by the Canadian armed forces, as well.
“The technology has caught up with the vision,” Rizzo says. But even still, he thinks VR has a long way to go before its true applications are tapped into. “It’s still in the Model T phase,” he said.
At Emory University, trials with a new program in Bravemind are being conducted to help treat PTSD from sexual assault in the military. Rizzo says that’s a big issue he hopes can be treated with this new application.
Both Rizzo and Widerhold have hope that, through VR, some of the stigma can be taken out of mental health and seeking treatment. By viewing VR therapy as training, it will help normalize it. Rizzo hopes to see VR incorporated into various elements of the military activities, before and deployment, to help soldiers get re-adjusted more quickly.
At the VR Medical Center, Wiederhold says they working hard to figure out ways to bring virtual reality treatment out of the facility without sacrificing the quality of care provided by a therapist present. If patients need it, he sees teletherapy as a way to incorporate VR treatment more effectively in the home and extend the range of care.
This article appeared in an InsideHook newsletter. Sign up for free to get more on travel, wellness, style, drinking, and culture.